Testicular Cancer Self-Exam: Guide for Early Detection

A testicular self-exam is a crucial and straightforward method for early detection of testicular cancer, enabling timely medical intervention and significantly improving prognosis by allowing individuals to identify changes in their testicles.
Understanding how to perform a self-exam for testicular cancer: a simple guide for early detection is not just about a medical procedure; it’s about empowering yourself with knowledge and proactive health management. While often overshadowed by other health discussions, testicular cancer remains a significant concern for men, particularly younger individuals. This guide aims to demystify the process, offering clear, actionable steps that can integrate seamlessly into your routine, providing peace of mind and potentially life-saving insights.
Understanding testicular cancer: what you need to know
Testicular cancer, though relatively rare, is the most common cancer in American males aged 15 to 35. This demographic includes teenagers, young adults, and even men in their early thirties. Recognizing this highlights the importance of awareness and routine self-examinations among this particular age group. Unlike some other cancers that predominantly affect older populations, testicular cancer often strikes at a time in a man’s life when he is building a career, establishing relationships, and generally feeling invincible, making early detection even more critical for preserving quality of life.
The good news is that testicular cancer is highly curable, especially when detected early. Survival rates are exceptionally high, often exceeding 95% if caught in its initial stages. This remarkable success rate underscores why self-exams are not just a recommendation but a vital component of men’s health. The earlier a lump or abnormality is discovered, the simpler and less invasive the treatment tends to be, often involving less extensive surgery and fewer aggressive therapies.
Types and risk factors
There are several types of testicular cancer, but the vast majority are germ cell tumors, which originate in the cells that produce sperm. These are further divided into seminomas and non-seminomas. Seminomas tend to grow and spread more slowly, while non-seminomas can be more aggressive. Understanding the type helps doctors determine the best course of treatment. The distinction isn’t strictly necessary for a self-exam, but it’s valuable knowledge if a diagnosis is made.
While the exact causes of testicular cancer are not fully understood, several risk factors have been identified. One of the most significant is cryptorchidism, or undescended testicle, a condition where one or both testicles fail to move into the scrotum before birth. Even if corrected surgically, the risk remains higher. Other risk factors include a family history of testicular cancer, previous testicular cancer in the other testicle, and certain genetic conditions like Klinefelter syndrome.
- Cryptorchidism: Undescended testicle at birth significantly increases risk.
- Family History: Having a father or brother with testicular cancer elevates personal risk.
- Previous Cancer: If one testicle has had cancer, the other is at higher risk.
- Race and Ethnicity: White men, particularly those of Scandinavian descent, have a higher incidence rate compared to other racial groups.
It’s important to note that most men who develop testicular cancer do not have any of these known risk factors, reinforcing the message that self-exams are a universal recommendation for all men, regardless of their individual risk profile. While risk factors provide valuable context, they should not deter anyone from performing regular self-checks. The simplicity and effectiveness of a self-exam make it an invaluable tool for everyone.
Understanding these fundamental aspects of testicular cancer—its prevalence among young men, high curability rates with early detection, and key risk factors—lays a crucial foundation for appreciating the profound importance of self-examination. This knowledge empowers individuals to take charge of their health, moving beyond fear to proactive prevention and early intervention.
When and how often to perform a self-exam
The timing and frequency of testicular self-exams are crucial for their effectiveness. Consistency is key, as it allows individuals to become familiar with the normal feel of their testicles, making it easier to detect any changes. Establishing a regular routine ensures that potential abnormalities don’t go unnoticed for extended periods, maximizing the chances of early detection and successful treatment outcomes.
The recommended frequency for a testicular self-exam is generally once a month. Choosing a consistent time slot can help integrate it into your routine, much like brushing your teeth or showering. Many experts suggest performing the exam after a warm bath or shower. The warmth causes the scrotal skin to relax, making it easier to feel for any lumps or changes within the testicles. This relaxed state of the scrotum provides optimal conditions for a thorough and accurate examination.
Ideal timing for examination
- After a warm bath or shower: The heat relaxes the scrotum, making examination easier.
- Monthly on a specific date: Choose a memorable date, like the first or last day of the month, to ensure consistency.
- During a relaxed, private moment: Ensure you are undisturbed to focus fully on the examination.
Picking a specific day each month can help you remember to perform the exam. For instance, you might choose the first day of every month, or perhaps a birthday or anniversary date (not necessarily your own, but one you can easily recall). This consistency builds a habit, reducing the likelihood of skipping exams and increasing the probability of detecting subtle changes over time. When it becomes a routine, it no longer feels like a chore but a natural part of personal hygiene and health maintenance.
Regularity is not just about remembering to do it, but also about building a mental “map” of what your testicles normally feel like. Each person’s anatomy is unique, and what feels normal for one individual might be different for another. By performing monthly exams, you develop a personal baseline, making any deviation from this norm more apparent. It’s this familiarity that empowers you to distinguish between normal structures and concerning abnormalities, such as new lumps or changes in size or texture.
Developing a routine and maintaining awareness
While monthly exams are the standard, maintaining general awareness of your body is also important. If you notice anything unusual between scheduled exams, don’t wait for your next check-in; consult a doctor immediately. This continuous vigilance is particularly crucial because, while testicular cancer is often slow-growing, prompt action is always beneficial. The goal is to catch any changes as soon as they occur, ensuring the quickest possible medical evaluation.
It’s also wise to discuss self-exams with a healthcare provider during routine physicals. They can offer guidance, demonstrate the correct technique, and address any concerns you might have. This professional input can reinforce your confidence in performing the exam correctly and interpret your findings. Sometimes, learning directly from a medical professional can alleviate anxieties and clarify any ambiguities about what you should be feeling for.
By making the testicular self-exam a regular, comfortable, and private part of your personal care routine, you are taking a significant step towards safeguarding your health. The time invested—just a few minutes each month—is minimal compared to the enormous potential benefit of early cancer detection. This proactive approach ensures that you are consistently monitoring your body and acting swiftly if any changes arise, ultimately promoting long-term well-being and peace of mind.
Step-by-step guide to performing the self-exam
Performing a testicular self-exam is a simple process that takes only a few minutes, yet it can be immensely effective in detecting early signs of testicular cancer. The key is to be gentle, thorough, and aware of the normal feel of your testicles. This step-by-step guide walks you through the procedure, ensuring you cover all the necessary areas and identify any potential anomalies with confidence and precision.
Preparation and positioning
Begin by standing in front of a mirror. This allows you to visually inspect the scrotum for any changes in skin texture, swelling, or discolouration. While visual inspection is helpful, the manual examination is the primary method for detecting lumps. As mentioned, the ideal time is after a warm bath or shower, as the relaxed scrotal skin makes the testicles more accessible and easier to observe and feel.
Hold your penis out of the way. Then, take one testicle at a time between your thumbs and fingers. It’s important to examine each testicle individually to ensure a thorough check of its entire surface. This systematic approach prevents you from missing any areas and helps you differentiate between different structures within the scrotum. The testicles should feel roughly oval-shaped and smooth.
The examination technique
Gently roll the testicle between your thumbs and fingers. Use light pressure, but enough to feel the entire surface. Start at the top of the testicle and move downwards, covering all sides. The goal is to feel for any hard lumps, smooth rounded bumps, or changes in the size, shape, or consistency of the testicle. Pay attention to any areas of tenderness or pain that were not present before.
Behind each testicle, you will normally feel a soft, tube-like structure called the epididymis. This structure carries sperm from the testicle. It often feels like a small, soft cord or a collection of small tubes. It’s a normal part of the anatomy, so don’t mistake it for an abnormality. Above the epididymis, you’ll feel the vas deferens, a firm, smooth, and much larger tube that transports sperm. Becoming familiar with these normal structures will help you distinguish them from any suspicious lumps.
- Roll gently: Use both thumbs and fingers, covering the entire surface of each testicle.
- Feel for abnormalities: Look for hard lumps, bumps, changes in size, shape, or consistency.
- Identify normal anatomy: Locate the epididymis (soft tube behind) and vas deferens (firmer tube above).
- Repeat on both sides: Ensure each testicle is thoroughly examined in the same manner.
Once you have thoroughly examined one testicle, repeat the process for the other. It’s common for one testicle to be slightly larger or hang lower than the other; this is generally normal. The key is to notice any new changes in either testicle, not necessarily absolute symmetry between the two.
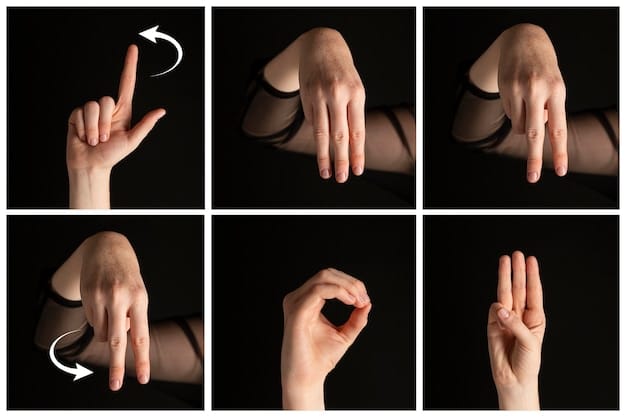
It can be helpful to visualize the testicle as a globe and systematically explore its ‘surface’ area by area, ensuring no part is left unchecked. This method ensures that bumps or lumps, even if small or subtly located, are not overlooked. The more familiar you become with your own anatomy through regular self-exams, the quicker you will be able to notice any deviations from your personal norm.
Remember, the purpose of the self-exam is early detection. If you find anything unusual, it does not automatically mean you have cancer. Many lumps are benign cysts or harmless conditions. However, any suspicious finding warrants immediate medical attention from a healthcare provider. They can properly diagnose the issue and provide appropriate guidance and care, ensuring your peace of mind and health.
What to look and feel for: identifying abnormalities
The success of a testicular self-exam lies in knowing what to look and feel for. While most men are familiar with the basic anatomy, recognizing an abnormality requires a keen sense of touch and visual observation, combined with an understanding of what constitutes a deviation from normal. It’s not just about finding a lump; it’s about identifying changes in size, shape, consistency, or the presence of discomfort.
The most common sign of testicular cancer is a painless lump or swelling in either testicle. This lump might vary in size, from as small as a pea to much larger. It can feel firm or hard, and it might be located anywhere on the testicle itself, distinct from the normal soft tube of the epididymis at the back. While usually painless, some lumps can cause a dull ache in the groin or scrotum, or a feeling of heaviness.
Key indicators of concern
- Painless lump or swelling: The most common symptom, varying in size and firmness.
- Change in size or shape: One testicle growing or shrinking, or becoming misshapen.
- Feeling of heaviness: A sensation of weight in the scrotum.
- Dull ache in the groin or scrotum: Persistent, low-level discomfort.
- Sudden collection of fluid in the scrotum: Though often benign, it warrants investigation.
- Pain or discomfort in the testicle or scrotum: Any new or persistent pain.
Beyond a distinct lump, other signs can indicate a potential problem. A general enlargement or shrinkage of a testicle without a specific lump can be a symptom. Sometimes, the consistency of the testicle changes; it might feel firmer or softer than usual. These subtle textural changes are why familiarity with your normal anatomy is paramount. Only by regular self-exams can you gauge what is typical for your body.
A feeling of heaviness in the scrotum, even without a noticeable lump, sometimes indicates an underlying issue. This sensation is often described as a dragging feeling. Similarly, a dull ache in the lower abdomen or groin area, or even in the scrotum, might be a symptom. While many benign conditions can cause these sensations, their persistence or new onset warrants medical evaluation.
It’s important to remember that not all lumps or changes mean cancer. Many benign conditions can affect the testicles, such as:
Among the most common are epididymal cysts, which are fluid-filled sacs in the epididymis and are harmless. Varicoceles, which are varicose veins in the scrotum, can feel like a “bag of worms” and are often benign, though they can sometimes affect fertility. Hydroceles are fluid collections around the testicle that cause swelling but are typically not cancerous. These conditions are common and usually diagnosed with an ultrasound.
However, differentiating between benign conditions and potentially malignant ones requires professional medical expertise. Therefore, the moment you notice any change, whether it’s a lump, swelling, change in consistency, pain, or discomfort, it is crucial to consult a healthcare provider. Do not try to self-diagnose based on information found online. Only a doctor can accurately assess your symptoms, perform necessary tests (such as an ultrasound or blood tests), and provide a definitive diagnosis, ensuring you receive appropriate and timely care.
The self-exam is merely a screening tool. Its purpose is to alert you to changes that an expert needs to examine further. Your proactive approach in noticing these changes is a critical step in safeguarding your health, significantly improving outcomes if any serious condition is indeed present.
When to see a doctor: next steps after finding an abnormality
Discovering an abnormality during a testicular self-exam can be a source of anxiety, but it’s crucial to remain calm and understand that most changes are not cancerous. However, any new lump, swelling, pain, or change in the testicle’s size or consistency warrants immediate medical attention. Your prompt action is key to a swift diagnosis and effective treatment, regardless of the underlying cause.
The first and most important step after noticing something unusual is to schedule an appointment with a healthcare provider. This could be your primary care physician, a urologist (a doctor specializing in conditions of the urinary tract and male reproductive system), or a general practitioner. Do not postpone this visit, even if the change seems minor or you believe it might be benign. Early consultation ensures that if it is cancer, treatment can begin sooner, which significantly improves the prognosis.
What to expect during a medical consultation
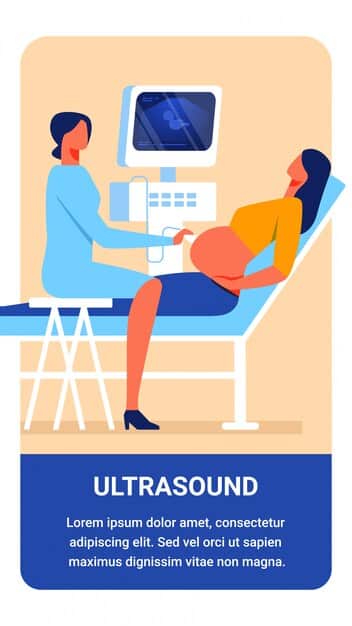
During your appointment, the doctor will likely perform a physical examination of your testicles, similar to your self-exam but with professional expertise. They will feel for lumps, swelling, and tenderness. They might also dim the lights and shine a small light through your scrotum (transillumination) to see if the lump is solid or filled with fluid. Fluid-filled lumps (like hydroceles) often glow, whereas solid masses (like tumors) do not.
If the doctor finds anything suspicious during the physical exam, they will probably recommend further diagnostic tests. The most common and effective initial test is an ultrasound of the scrotum. This is a non-invasive imaging test that uses sound waves to create detailed images of the testicles and surrounding structures. An ultrasound can typically determine whether a mass is solid (potentially cancerous) or fluid-filled (usually benign).
- Physical Examination: Doctor will manually examine the scrotum.
- Ultrasound: Non-invasive imaging to differentiate solid from fluid-filled masses.
- Blood Tests: To check for tumor markers if cancer is suspected.
- Biopsy (rare for diagnosis): Usually done after surgical removal, not beforehand.
Additionally, blood tests might be ordered to check for tumor markers. These are substances produced by cancer cells or by other cells in response to cancer. Elevated levels of certain markers, such as alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG), can indicate the presence of testicular cancer. However, it’s important to note that not all testicular cancers produce these markers, and elevated levels can sometimes be due to other conditions.
In most cases, if a solid mass is identified and cancer is strongly suspected, the next step is often surgical removal of the testicle (orchiectomy). Unlike many other cancers, a biopsy (removing a small piece of tissue for examination) is rarely performed on a suspicious testicular mass before surgery. This is because a biopsy can disrupt the tumor and potentially spread cancer cells. The removed testicle is then sent to a pathologist for microscopic examination to confirm the diagnosis and determine the type of cancer, guiding further treatment decisions.
Receiving feedback from your healthcare provider, whether it’s reassurance that the finding is benign or a confirmed diagnosis, is vital. If it is cancer, early detection significantly improves treatment success rates, which often exceed 95% for early-stage cases. Your proactive self-exam and timely medical consultation are powerful tools in your health arsenal, giving you the best possible outcome.
Trust your instincts. If something doesn’t feel right, get it checked. It’s always better to be safe than sorry when it comes to your health. Your diligence in performing self-exams and seeking professional advice demonstrates a commendable commitment to your well-being.
Maintaining testicular health: beyond self-exams
While testicular self-exams are a cornerstone of early detection for testicular cancer, maintaining overall testicular health extends beyond this monthly check. A holistic approach encompasses general health practices, lifestyle choices, and being aware of other potential issues that can affect these vital organs. It’s about proactive care that promotes well-being and prevents a range of conditions.
General health practices play a significant role. A balanced diet rich in fruits, vegetables, and lean proteins provides essential nutrients for cellular health and general bodily function. Regular physical activity helps maintain a healthy weight, improves circulation, and contributes to overall vitality. Avoiding smoking and excessive alcohol consumption also reduces risks for various cancers and other health problems throughout the body.
Lifestyle and protective measures
Protecting the testicles from injury is also important. This is particularly relevant for individuals participating in sports or activities that expose the groin area to potential impact. Wearing appropriate athletic cups during contact sports can prevent blunt trauma that might lead to pain, swelling, or more serious injury. While injuries do not directly cause testicular cancer, severe trauma can lead to other complications that warrant medical attention.
Beyond cancer, other conditions can affect testicular health. These include:
- Infections: Epididymitis (inflammation of the epididymis) and orchitis (inflammation of the testicle) can be caused by bacterial or viral infections. Symptoms include pain, swelling, and fever. Prompt medical attention is necessary to prevent complications.
- Torsion: Testicular torsion is a medical emergency where the spermatic cord twists, cutting off blood supply to the testicle. It causes sudden, severe pain and requires immediate surgery to save the testicle. It’s more common in adolescents but can occur at any age.
- Hydroceles & Spermatoceles: These are fluid-filled sacs that can cause scrotal swelling but are generally benign and often don’t require treatment unless they become very large or symptomatic.
- Varicoceles: Enlarged veins in the scrotum, often described as feeling like a “bag of worms.” They are usually harmless but can sometimes cause discomfort or contribute to infertility.
Regular check-ups with a primary care physician are vital for overall health management, including discussions about testicular health. During these appointments, you can raise any concerns you have, discuss your self-exam findings, and receive professional guidance on any aspect of your reproductive health. These visits also allow for routine screenings for other health conditions that may not be apparent through self-exams.
Being attentive to symptoms beyond just lumps is also critical. Persistent pain, discomfort, changes in sexual function, or issues with urination should always prompt a visit to a doctor. These symptoms could indicate a range of conditions, from infections to prostate issues, and require professional diagnosis.
In essence, maintaining testicular health is about adopting a proactive, informed, and holistic approach to your well-being. By combining diligent self-exams, general healthy living, protection against injury, and regular medical check-ups, you equip yourself with the best possible defence against potential health issues. This comprehensive strategy not only focuses on prevention and early detection of serious conditions like cancer but also ensures the ongoing health and function of your reproductive system.
Empowering yourself through knowledge and action
The journey towards optimal sexual wellness and general health is a continuous one, defined by awareness, proactive engagement, and timely action. When it comes to something as critical as testicular cancer, empowering oneself through knowledge and consistent self-care can make an indelible impact. This guide has aimed to equip you with the essential tools and understanding needed to approach testicular health with confidence and vigilance.
The core message remains clear: a regular, properly performed testicular self-exam is a powerful, non-invasive method for early detection. It takes mere minutes each month, yet its potential to save lives or significantly improve treatment outcomes is immeasurable. By consistently checking your own body, you develop an intimate understanding of what is normal for you, making any deviation instantly noticeable. This personal familiarity is your first and most effective line of defense against testicular cancer.
However, the self-exam is not a diagnostic tool; it is a screening tool. Its purpose is to signal when professional medical attention is needed. Upon discovering any lump, swelling, pain, or change in consistency, the immediate next step is to consult a healthcare provider. Delay can be detrimental, and prompt professional evaluation ensures an accurate diagnosis and appropriate course of action. Remember, most findings are benign, but only a doctor can provide that reassurance or initiate necessary treatment.
Beyond self-exams, remember that overall health and lifestyle choices contribute to testicular well-being. A balanced diet, regular exercise, protection from injury, and routine general health check-ups all play a part in maintaining the vitality of your reproductive system. Being mindful of other symptoms, such as persistent pain or changes in bodily function, also informs a comprehensive approach to health management.
Ultimately, taking charge of your health means being informed, proactive, and responsible. It means understanding the importance of routine checks, being attuned to your body’s signals, and seeking expert advice when necessary. By integrating this knowledge into your life, you are not just preventing potential health crises; you are investing in a healthier, more confident future. Embrace this power of self-care and knowledge, knowing that you are taking significant steps to safeguard your well-being.
| Key Point | Brief Description |
|---|---|
| 🗓️ Monthly Exam | Perform self-exams monthly after a warm shower for best results and consistency. |
| 🔍 What to Feel For | Check for painless lumps, swelling, changes in size/shape, or feelings of heaviness. |
| 👨⚕️ Seek Medical Help | Consult a doctor immediately if any abnormality is detected; early action is crucial. |
| 🌟 High Cure Rate | Testicular cancer is highly curable, especially when detected and treated early. |
Frequently asked questions about testicular self-exams
It is recommended to perform a testicular self-exam once a month. Regularity helps you become familiar with the normal feel of your testicles, making it easier to notice any changes. Performing it after a warm shower or bath is ideal, as the relaxed scrotal skin allows for a more thorough examination and easier detection of potential abnormalities.
During a testicular self-exam, you should be looking and feeling for any new lumps (which may or may not be painful), swelling, changes in the size or shape of either testicle, or a feeling of heaviness in the scrotum. Also, pay attention to any new or persistent pain or discomfort. Familiarize yourself with the normal structures like the epididymis and vas deferens to avoid confusion.
Yes, it is completely normal for one testicle to be slightly larger or hang lower than the other. This anatomical variation is common among men and typically does not indicate any health issue. The key is to recognize what is normal for your body and to identify any new or unusual changes that occur over time, rather than comparing absolute sizes.
No, finding a lump does not automatically mean you have cancer. Many lumps or changes are benign and can be caused by conditions such as cysts, infections, or fluid collections. However, any new lump or abnormality should always be evaluated by a healthcare professional as soon as possible to get an accurate diagnosis and appropriate medical advice. Early consultation is crucial.
If you find anything unusual during your testicular self-exam, the most important step is to schedule an appointment with a healthcare provider immediately. Do not panic, but do not delay. Your doctor can perform a professional examination and order further tests, such as an ultrasound or blood tests, to determine the cause of the abnormality and provide a definitive diagnosis.
Conclusion
The journey towards proactive health management is driven by informed vigilance, and when it comes to male reproductive health, the testicular self-exam stands as a simple yet profoundly impactful practice. As we’ve explored, understanding the nuances of testicular cancer, the precise steps for self-examination, and the critical signs to look for are not merely academic exercises; they are vital components of personal responsibility. This guide has aimed to demystify the process, transforming it from a daunting task into an accessible, empowering routine. By consistently performing these checks, and by promptly seeking professional advice when necessary, every man has the power to significantly improve the prospects of early detection, ensuring that any potential health issue is addressed swiftly and effectively. Your commitment to these few minutes each month is a powerful investment in a healthier future.





