Navigating Sexual Health After Prostatectomy: A Recovery Guide

Navigating sexual health after prostatectomy involves understanding potential changes, exploring various recovery strategies, and embracing open communication with partners and healthcare providers to redefine intimacy and well-being.
Prostatectomy, a surgical procedure to remove all or part of the prostate gland, often brings profound relief for conditions like prostate cancer. However, for many men, it introduces significant concerns about their sexual health and intimacy. Understanding How to Navigate Sexual Health After a Prostatectomy: A Guide to Recovery and Intimacy becomes a crucial part of the post-operative journey, requiring patience, informed choices, and sometimes, the support of professionals.
Understanding the Impact of Prostatectomy on Sexual Function
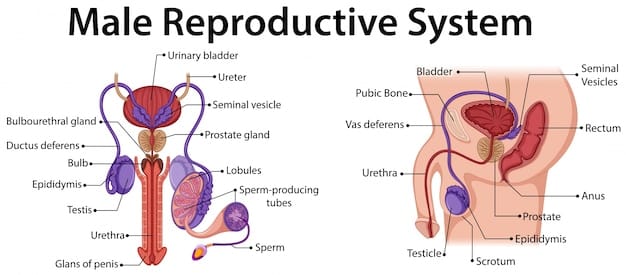
A prostatectomy, while life-saving for many, can significantly alter sexual function, primarily affecting erectile quality and ejaculatory habits. These changes are a direct consequence of the surgical removal of the prostate, an organ intricately involved in both urinary and sexual systems. Addressing these intimately personal changes requires a nuanced approach, acknowledging that recovery is a highly individual process.
The extent of sexual impact often depends on the type of prostatectomy performed. Nerve-sparing techniques, for instance, aim to preserve the delicate nerves essential for erections, though complete preservation isn’t always possible or advisable, particularly in aggressive cancers. Even when nerves are spared, they can be stretched or bruised during surgery, leading to temporary or prolonged erectile dysfunction.
Erectile Dysfunction (ED) Post-Surgery
Erectile dysfunction is perhaps the most commonly discussed sexual side effect following prostatectomy. It results from damage to the cavernous nerves that run along the sides of the prostate and control blood flow to the penis. While many men experience immediate ED, the recovery of erectile function is possible, albeit gradually, over months or even years.
- Damage to nerve bundles: Even with nerve-sparing surgery, the nerves can be affected.
- Reduced blood flow: Surgical trauma can temporarily impede blood flow crucial for erections.
- Psychological aspects: Anxiety and depression about sexual performance can exacerbate ED.
The journey towards regaining erectile function is complex, involving both physiological healing and psychological adjustment. Patience is paramount, as the nerves regenerate and adapt. Early intervention and rehabilitation strategies are often recommended to support this recovery process.
Changes in Ejaculation and Orgasm
Significant changes typically occur in ejaculation post-prostatectomy. Since the prostate gland produces seminal fluid, removing it leads to “dry orgasm,” meaning no semen is ejaculated. This alteration can be surprising and disheartening for some men and their partners, even if orgasmic sensation remains.
- Dry orgasm: Absence of seminal fluid during climax.
- Altered orgasmic sensation: Some men report a different, sometimes less intense, orgasmic experience.
- Loss of fertility: The procedure renders men infertile due to the absence of semen.
While the physical act of ejaculation changes, the capacity for orgasm often persists. Many men can still achieve gratification, although the sensation may feel different from pre-surgery experiences. Discussing these expected changes with a healthcare provider beforehand can help manage expectations and reduce distress.
In summary, understanding the physiological and psychological impacts of prostatectomy on sexual health is the first vital step. This knowledge empowers individuals to engage proactively in their recovery, seeking appropriate interventions and maintaining realistic expectations about the path ahead.
Early Intervention and Rehabilitation Strategies
The period immediately following a prostatectomy is critical for initiating strategies that can aid in the recovery of sexual function. Early intervention is often linked to better long-term outcomes, focusing on preserving penile health and stimulating nerve regeneration. These proactive measures can play a significant role in mitigating the severity of post-surgical sexual dysfunction and accelerating the healing process.

The concept of “penile rehabilitation” aims to facilitate the return of natural erections by encouraging blood flow to the penis, which helps to preserve tissue health and prevent atrophy. This often involves a multi-modal approach, combining various treatments tailored to the individual’s needs and recovery progress.
Penile Rehabilitation Programs
Penile rehabilitation often starts shortly after catheter removal and typically involves a combination of medication and devices. The goal is to encourage regular erections, which helps to oxygenate the penile tissues and prevent fibrosis, a process that can permanently impair erectile function.
- PDE5 Inhibitors: Medications like sildenafil (Viagra) or tadalafil (Cialis) are frequently prescribed to promote blood flow. They can be used daily at a lower dose or on demand.
- Vacuum Erection Devices (VEDs): These devices create a vacuum around the penis, drawing blood into the shaft and creating an erection. They are used to improve penile circulation and tissue health.
- Penile Injections: Medications like alprostadil, injected directly into the penis, can induce an erection for intercourse, providing a reliable alternative for some men.
Starting these therapies early, as advised by a urologist, is crucial. The aim is to “keep the penis alive” during the nerve healing phase. Consistency in use, even if full erections aren’t initially achieved, is often emphasized for optimal results.
Pelvic Floor Exercises (Kegels)
While often associated with urinary continence, pelvic floor exercises, or Kegels, also play a role in sexual health recovery. Strengthening these muscles can improve blood flow to the pelvic area and may enhance erectile quality and ejaculatory control (even in the absence of semen).
Proper technique is key for Kegel exercises. It involves identifying the correct muscles (the ones used to stop urine mid-stream or prevent passing gas) and then contracting and relaxing them rhythmically. A pelvic floor physical therapist can provide guidance and ensure the exercises are performed effectively.
Engaging in these exercises regularly can contribute to overall pelvic health and sexual function. They empower men to actively participate in their recovery process, fostering a sense of control and progress.
In essence, early intervention and consistent adherence to rehabilitation programs, including pharmacological treatments, devices, and physical exercises, are fundamental components of navigating sexual health after a prostatectomy. These strategies provide a framework for encouraging physiological recovery and supporting psychological well-being during this transformative period.
Medical and Therapeutic Options for Erectile Dysfunction
As recovery progresses following prostatectomy, many men will explore various medical and therapeutic options to address persistent erectile dysfunction. While early rehabilitation focuses on preparing the body for natural recovery, these longer-term solutions provide effective ways to restore satisfactory sexual function, offering hope and tangible improvements to quality of life. The choice of therapy often depends on the individual’s response to initial treatments, their preferences, and overall health status.
The landscape of ED treatments is diverse, ranging from oral medications to surgical implants, each with its own benefits, considerations, and potential side effects. A tailored approach, often guided by a urologist or sexual health specialist, is crucial for selecting the most appropriate and effective pathway.
Oral Medications and Beyond
Phosphodiesterase-5 (PDE5) inhibitors are typically the first-line pharmacotherapy for ED. While often initiated early for penile rehabilitation, they continue to be a cornerstone for on-demand use once some nerve function returns. If these don’t provide sufficient results, other options are available.
- PDE5 Inhibitors (e.g., Sildenafil, Tadalafil): Effective for many men by enhancing the effects of nitric oxide, a natural chemical that relaxes muscles in the penis and increases blood flow.
- Alprostadil (injections or urethral suppositories): Directly introduces a prostaglandin that causes vasodilation, leading to an erection. Used when oral medications are ineffective or contraindicated.
- Vacuum Erection Devices (VEDs): Can be used for intercourse as needed, providing a reliable erection by drawing blood into the penis.
Penile Implants (Prostheses)
For men with severe or refractory ED, for whom other treatments have failed or are unsuitable, a penile implant might be a viable option. This surgical procedure involves placing inflatable or malleable rods inside the penis, allowing for on-demand erections.
- Inflatable implants: Most common type, allowing an erection to be created and deflated. Offers a natural feel and discreet use.
- Malleable implants: Simple and always semi-rigid, allowing for positioning for sexual activity.
Penile implants have high satisfaction rates among users and their partners. They offer a permanent solution that bypasses nerve damage, providing a reliable and spontaneous way to achieve erections. However, it’s an irreversible surgical procedure, and discussion with a specialist about risks and benefits is essential.
Navigating the options for ED treatment requires open dialogue with healthcare providers. It’s a journey of finding what works best, balancing effectiveness with personal comfort and lifestyle. The goal is to restore not just function, but also confidence and satisfaction in sexual intimacy.
Redefining Intimacy and Communication
Beyond the physical aspects of sexual function, prostatectomy can deeply impact intimacy and emotional connection within relationships. Redefining intimacy post-surgery is a crucial, often overlooked, component of recovery. It requires open, honest communication between partners, a willingness to explore new ways of connecting, and an understanding that intimacy extends far beyond penetrative sex. This emotional landscape is as significant as the physical one.
Many couples face challenges related to body image, performance anxiety, and changed expectations. Addressing these issues with empathy and patience can transform potential obstacles into opportunities for deeper connection and mutual understanding. The journey is not just about healing the body, but also nurturing the relationship.
Open Dialogue with Your Partner
The cornerstone of redefining intimacy is candid communication. Both partners need to feel comfortable expressing their feelings, fears, and desires without judgment. This means talking about changes in sexual function, emotional impacts, and exploring what intimacy means to both of them now.
- Share feelings: Discuss anxieties, frustrations, and hopes openly.
- Reaffirm affection: Emphasize that love, attraction, and desire for intimacy remain.
- Discuss expectations: Align on what realistic sexual activity might look like, and explore new forms of pleasure.
Scheduling dedicated, calm conversations can be helpful, similar to how one might approach discussing other significant life changes. It’s about building a shared understanding and supporting each other through discomfort and uncertainty.
Exploring New Forms of Intimacy
With traditional intercourse potentially altered, couples have the opportunity to explore a broader spectrum of intimate activities. This can lead to a richer, more diverse sexual experience that is less focused on performance and more on connection and pleasure.
Intimacy encompasses far more than just penetrative sex. It includes emotional closeness, physical affection, shared experiences, and mutual pleasure. After prostatectomy, couples can rediscover intimacy through:
- Non-penetrative sexual activities: Oral sex, manual stimulation, using sex toys, and mutual masturbation can provide pleasure and closeness.
- Affirming physical touch: Cuddling, kissing, massage, and prolonged embrace can deepen emotional bonds.
- Emotional connection: Sharing vulnerabilities, spending quality time, and engaging in shared interests reinforces a loving partnership.
Embracing these alternative pathways to intimacy can alleviate pressure and foster a more expansive view of sexual expression. It’s an invitation to creativity and mutual discovery, strengthening the relationship in unexpected ways. Redefining intimacy is a continuous process of adaptation, growth, and shared exploration, reinforcing that a fulfilling sexual life is possible beyond traditional norms even after significant surgical changes.
Psychological and Emotional Support
The journey after a prostatectomy is not only physical but also profoundly psychological and emotional. Many men experience feelings of loss, anxiety, depression, and a significant blow to their self-esteem due to changes in body image and sexual function. Addressing these mental health aspects is as vital as managing the physical symptoms for overall recovery and well-being. Recognizing the need for such support is the first step towards healing the unseen wounds.
Ignoring the emotional toll can hinder physical recovery and strain relationships. Creating a supportive environment, both personally and professionally, is essential for navigating this complex emotional landscape. It allows individuals to process their experiences, adjust to new realities, and rebuild their confidence.
Individual and Couples Counseling
Professional psychological support can provide invaluable tools and strategies for coping with the emotional challenges post-prostatectomy. Therapy offers a safe space to explore feelings, develop coping mechanisms, and process grief or anxiety related to changes in health and identity.
- Individual therapy: Helps men process feelings of loss, anxiety about performance, shifts in identity, and depression. A therapist can provide validation and strategies for self-care.
- Couples counseling: Facilitates communication between partners, addresses shared anxieties, and helps redefine intimacy together. It can prevent misunderstandings and strengthen the relationship bond.
Seeking therapy is a sign of strength, not weakness. It can significantly improve emotional resilience and facilitate a smoother adaptation to life after surgery. A skilled therapist can guide discussions on sensitive topics, ensuring both partners feel heard and supported.
Support Groups and Peer Networks
Connecting with others who have undergone similar experiences can be incredibly validating and empowering. Support groups offer a unique opportunity to share stories, exchange practical advice, and realize that one is not alone in their struggles. This sense of community can reduce feelings of isolation and provide a powerful source of emotional strength.
Peer networks, whether online or in-person, allow men to learn from those further along in their recovery journey. Hearing about different strategies, successes, and challenges from peers can offer new perspectives and motivate individuals to persist in their own recovery efforts.
- Shared experiences: Reduces feelings of isolation and normalizes challenges.
- Practical advice: Peers can offer tips on managing side effects or navigating relationships based on their own lived experiences.
- Emotional validation: Provides a space where feelings are understood and accepted without judgment.
Engaging in psychological and emotional support is not merely about coping; it’s about actively building resilience and fostering a positive outlook. By addressing these aspects comprehensively, men can achieve a more holistic recovery, improving their overall quality of life and strengthening their relationships.
Long-Term Management and Lifestyle Adjustments
Life after prostatectomy is a journey of ongoing adjustment, and long-term management plays a critical role in sustaining sexual health and overall well-being. This involves a continuous commitment to lifestyle choices, medical follow-ups, and adapting to changes as they evolve over time. The goal is not just to recover but to thrive, ensuring that sexual health remains a cherished and manageable aspect of life for years to come.
Maintaining a holistic approach, which includes physical health, mental resilience, and open relationships, is key to navigating the post-prostatectomy landscape successfully. This section explores strategies for integrating sexual health management into daily life.
Maintaining Overall Health
General health significantly impacts sexual function. Adhering to a healthy lifestyle benefits cardiovascular health, which is crucial for erectile function. Weight management, a balanced diet, and regular physical activity can all contribute positively.
- Healthy diet: Focus on nutrient-rich foods, reduce processed items.
- Regular exercise: Improves blood circulation, energy levels, and mood.
- Smoking cessation and alcohol moderation: Contributes to better cardiovascular health and overall physical well-being.
These lifestyle choices not only support sexual health but also contribute to a better quality of life. They are controllable factors that empower individuals to take an active role in their ongoing recovery and health maintenance.
Ongoing Medical Follow-up and Adjustments
Regular check-ups with a urologist or sexual health specialist are essential for monitoring progress, adjusting treatment plans as needed, and addressing any new concerns. Recovery is dynamic, and what works today might need adjustment tomorrow.
This includes:
- Monitoring ED treatments: Adjusting dosages, trying different medications, or exploring new therapies as appropriate.
- Addressing other side effects: Managing urinary incontinence or bowel issues, which can also impact quality of life and sexual confidence.
- Psychological check-ins: Discussing emotional well-being and seeking referrals for counseling if persistent issues arise.
The ongoing dialogue with healthcare providers ensures that interventions remain aligned with current needs and advances in medical knowledge. It’s a partnership aimed at maximizing function and satisfaction.
Moreover, embracing adaptability is crucial for long-term sexual health. Understanding that intimacy may evolve and finding joy in new forms of connection can foster a resilient and fulfilling sexual life. This continuous journey of learning, adjusting, and self-care is fundamental to achieving sustained well-being and satisfaction post-prostatectomy.
| Key Aspect | Brief Description |
|---|---|
| 💡 Understanding Impact | Recognize changes in ED, ejaculation, and orgasm for informed recovery. |
| 🌱 Rehabilitation Strategies | Start early with penile rehab (meds, VEDs) and Kegel exercises. |
| 💬 Redefining Intimacy | Open communication and exploring alternative forms of intimacy are key. |
| 🧠 Emotional Support | Seek counseling or support groups for psychological and emotional well-being. |
Frequently Asked Questions About Sexual Health Post-Prostatectomy
Many men do recover erectile function after prostatectomy, especially with nerve-sparing techniques and comprehensive penile rehabilitation. Recovery can take months to years, varying by individual and surgical details. Early and consistent intervention with medications or devices significantly improves the chances of regaining satisfactory erections.
A “dry orgasm” means experiencing climax without ejaculating semen, as the prostate and seminal vesicles (which produce seminal fluid) are removed. The physical sensation of orgasm typically remains, though it might feel different—some describe it as less forceful or intense. It’s a common and expected outcome of the surgery.
Open and honest communication with your partner is critically important. Discussing changes in sexual function, emotions, and intimacy helps manage expectations, reduce anxiety, and foster mutual understanding. It allows both partners to explore and redefine intimacy together, strengthening the emotional bond and finding new ways to connect sexually and emotionally.
Yes, several non-surgical options exist beyond oral medications for erectile dysfunction. These include vacuum erection devices (VEDs), which create an erection by drawing blood into the penis, and penile injections of medication like alprostadil, which can induce a reliable erection for intercourse. A urologist can help determine the most suitable option.
Psychological support can be found through individual or couples counseling with a therapist specializing in sexual health or cancer recovery. Support groups, either in-person or online, also provide a valuable platform for sharing experiences and receiving peer support. Discussing these needs with your urologist can often lead to helpful referrals.
Conclusion
Navigating sexual health after a prostatectomy is undeniably a complex journey, but one that is rich with possibilities for recovery, adaptation, and deeper intimacy. It requires a blend of medical intervention, proactive rehabilitation, open communication with partners, and essential psychological support. While the immediate aftermath may present challenges, understanding the potential impacts and proactively engaging with available solutions can significantly improve outcomes. Embracing a holistic approach—prioritizing physiological healing, fostering emotional resilience, and redefining intimacy—allows individuals to not only manage the changes but also discover new, fulfilling dimensions of their sexual and emotional well-being. The path forward is one of informed choices, patience, and a commitment to nurturing both personal health and cherished relationships.