Male Infertility Testing: A Comprehensive Guide for US Patients

Male infertility testing involves a series of evaluations to determine the causes of infertility in men, including semen analysis, physical exams, and hormone testing, helping to identify potential treatment options and improve chances of conception.
Embarking on the journey of fertility testing can be daunting, especially when it comes to male infertility. Understanding what to expect during male infertility testing is crucial for navigating the process with confidence and making informed decisions about your reproductive health.
Understanding Male Infertility: An Overview
Infertility is often perceived as a female issue, but male factors contribute significantly to couples struggling to conceive. Understanding the causes and the available testing methods is the first step in addressing the challenges of male infertility.
Common Causes of Male Infertility
Male infertility can stem from a variety of factors, ranging from genetic conditions to lifestyle choices. Identifying the root cause is essential for targeted treatment.
- Sperm Disorders: Issues with sperm count, motility (movement), and morphology (shape) are common culprits.
- Hormonal Imbalances: Hormones like testosterone play a crucial role in sperm production. Imbalances can disrupt this process.
- Structural Problems: Varicoceles (enlarged veins in the scrotum) and other structural issues can affect sperm production and delivery.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and obesity can negatively impact sperm quality.
Addressing these causes often involves a combination of medical treatments, lifestyle changes, and assisted reproductive technologies.
Initial Steps: The Physical Exam and Medical History
The first steps in male infertility testing often involve a thorough physical examination and a detailed review of your medical history. This helps the doctor gain an overall understanding of your health and identify potential contributing factors.
During the physical exam, the doctor will assess your general health, check for any physical abnormalities in the reproductive organs, and evaluate signs of hormonal imbalances. Your medical history will cover past illnesses, surgeries, medications, and lifestyle habits. This comprehensive assessment sets the stage for more specific tests.
Understanding your medical background and undergoing a physical exam are crucial starting points for diagnosing male infertility.

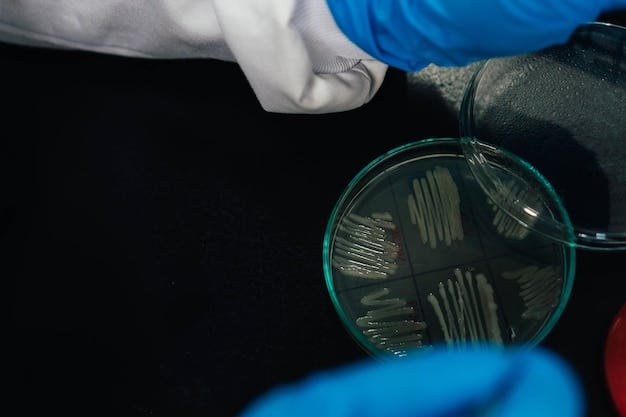
Semen Analysis: The Cornerstone of Male Infertility Testing
Semen analysis is a fundamental test that evaluates the quality and quantity of sperm. It provides valuable insights into a man’s fertility potential.
The test involves collecting a semen sample, typically through masturbation, after a period of abstinence (usually 2-3 days). The sample is then analyzed in a laboratory for several key parameters:
Key Parameters Evaluated in Semen Analysis
Semen analysis assesses several crucial factors that determine sperm health and fertility potential.
- Sperm Count: The number of sperm per milliliter of semen. A low sperm count (oligospermia) can reduce the chances of fertilization.
- Sperm Motility: The percentage of sperm that are moving and their ability to swim effectively. Poor motility (asthenospermia) hinders sperm from reaching the egg.
- Sperm Morphology: The shape and structure of sperm. Abnormal morphology (teratospermia) can affect the sperm’s ability to fertilize the egg.
- Semen Volume: The amount of semen produced. Low volume can indicate a blockage or other issues.
Understanding these parameters is essential for interpreting semen analysis results and determining the next steps in fertility evaluation.
Hormone Testing: Investigating Hormonal Imbalances
Hormones play a vital role in sperm production and overall reproductive health. Hormone testing can help identify imbalances that may be contributing to male infertility.
The most common hormone tests for male infertility include:
- Testosterone: The primary male sex hormone, essential for sperm production. Low levels can indicate hypogonadism.
- FSH (Follicle-Stimulating Hormone): Stimulates sperm production in the testicles. High levels can indicate testicular damage or failure.
- LH (Luteinizing Hormone): Stimulates testosterone production. Abnormal levels can disrupt hormonal balance.
- Prolactin: High levels can interfere with testosterone production and sperm function.
Hormone testing, combined with other evaluations, provides a comprehensive assessment of male reproductive health, guiding treatment decisions for optimizing fertility.
Genetic Testing: Exploring Genetic Factors in Male Infertility
Genetic factors can play a significant role in male infertility. Genetic testing can help identify specific genetic abnormalities that may be affecting sperm production or function.
Here’s what you should know about genetic testing in the context of male infertility:
Common Genetic Tests for Male Infertility
Several genetic tests can shed light on potential genetic causes of male infertility.
- Karyotype Analysis: Examines the chromosomes for abnormalities like Klinefelter syndrome (XXY), which can cause infertility.
- Y-Chromosome Microdeletion Testing: Detects deletions on the Y chromosome, which can affect sperm production.
- CFTR Mutation Testing: Screens for mutations in the CFTR gene, associated with congenital absence of the vas deferens (CAVD), a condition that can cause obstructive azoospermia.
Genetic testing provides valuable information for understanding and managing male infertility, helping couples make informed decisions about their reproductive options.
Advanced Diagnostic Procedures: When More Information Is Needed
In some cases, initial tests may not provide a complete picture of the cause of male infertility. Advanced diagnostic procedures can offer more detailed insights.
These procedures may include:
- Testicular Biopsy: Involves removing a small sample of testicular tissue for microscopic examination. It can help determine if sperm production is occurring normally.
- Vasography: An imaging technique used to visualize the vas deferens and identify any blockages.
- Transrectal Ultrasound: Used to examine the prostate and seminal vesicles, identifying potential abnormalities that may affect fertility.
These advanced tests are typically reserved for cases where initial evaluations are inconclusive or when specific issues are suspected.
Preparing for Male Infertility Testing: What to Expect
Preparing for male infertility testing involves understanding the process and following specific guidelines to ensure accurate results. Knowing what to expect can help alleviate anxiety and optimize the testing experience.
Practical Tips for Preparing for Testing
Proper preparation is crucial for accurate and reliable male infertility testing results.
- Abstinence: Follow the recommended period of abstinence (usually 2-3 days) before providing a semen sample.
- Medication Disclosure: Inform your doctor about all medications you are taking, as some drugs can affect sperm quality.
- Lifestyle Considerations: Avoid smoking, excessive alcohol consumption, and exposure to toxins before testing.
- Emotional Support: Seek emotional support from your partner, family, or a counselor to cope with the stress of fertility testing.
By following these tips and maintaining open communication with your healthcare provider, you can navigate male infertility testing with confidence and clarity.
| Key Point | Brief Description |
|---|---|
| 🔬 Semen Analysis | Evaluates sperm count, motility, and morphology. |
| 🧪 Hormone Testing | Checks testosterone, FSH, and LH levels. |
| 🧬 Genetic Testing | Identifies genetic factors affecting fertility. |
| 🩺 Physical Exam | Initial assessment for physical abnormalities. |
Frequently Asked Questions (FAQ)
▼
The first step typically involves a physical exam and a review of your medical history by a healthcare provider to identify potential factors contributing to infertility.
▼
It is generally recommended to abstain from sexual activity for 2-3 days before providing a semen sample to ensure accurate results, but avoid abstaining for longer than 7 days.
▼
A low sperm count (oligospermia) may indicate hormonal imbalances, structural issues, lifestyle factors, or genetic conditions affecting sperm production.
▼
Yes, lifestyle changes such as quitting smoking, reducing alcohol consumption, maintaining a healthy weight, and avoiding toxins can positively impact sperm quality and male fertility.
▼
Treatment options include medication, surgery (e.g., varicocelectomy), assisted reproductive technologies (ART) like IVF/ICSI, and lifestyle modifications to address the underlying causes of infertility.
Conclusion
Navigating male infertility testing can feel overwhelming, but understanding the process and available options empowers you to take proactive steps towards improving your reproductive health. From initial physical exams and semen analysis to hormone and genetic testing, each evaluation plays a crucial role in identifying the underlying causes of infertility and guiding appropriate treatment strategies to enhance your chances of conception.





