Long-Term Effects of Steroid Use on Male Sexual Health
Long-term anabolic steroid use in men can profoundly impact sexual health, leading to conditions like hypogonadism, erectile dysfunction, infertility, and psychological issues, due to the disruption of natural hormonal balance.
Understanding what are the long-term effects of steroid use on male sexual health is crucial for anyone considering or currently using these substances. The appeal of enhanced physique and athletic performance often overshadows the serious, often irreversible, consequences hidden beneath the surface. This article delves into the science, the stories, and the stark realities of how prolonged steroid use can dismantle a man’s most intimate well-being.
the allure and the anatomy of anabolic steroids
Anabolic-androgenic steroids (AAS) are synthetic variations of the male sex hormone testosterone. Their primary appeal lies in their ability to promote muscle growth (anabolic effects) and the development of male characteristics (androgenic effects). For decades, they have been misused by athletes, bodybuilders, and individuals seeking to alter their physical appearance, often under the misguided belief that the benefits outweigh the risks. However, the human body is a finely tuned machine, and introducing exogenous hormones at supraphysiological levels inevitably triggers a cascade of effects, many of which are detrimental, particularly concerning sexual health.
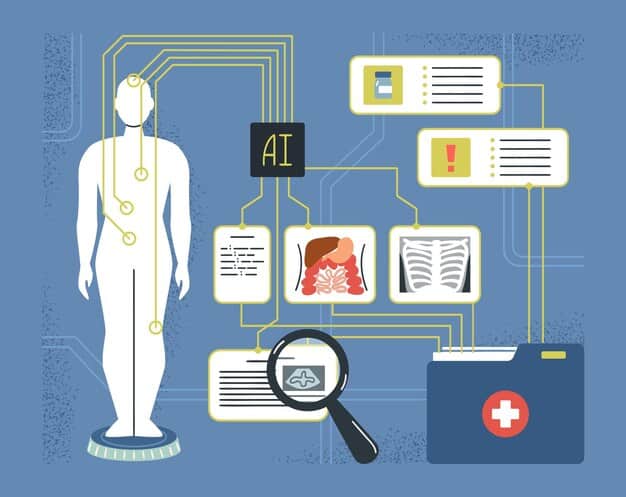
When an individual administers AAS, the body’s natural hormonal feedback loop is disrupted. The hypothalamus-pituitary-gonadal (HPG) axis, responsible for regulating testosterone production, perceives the high levels of synthetic testosterone and responds by shutting down its own production. This suppression is a core mechanism behind many of the long-term sexual health issues associated with steroid abuse. The body attempts to maintain homeostasis, but the artificial influx of hormones overwhelms this delicate balance.
the hpg axis and its disruption
The HPG axis is a sophisticated endocrine system involving signals between the hypothalamus, the pituitary gland, and the gonads (testes in males). The hypothalamus releases gonadotropin-releasing hormone (GnRH), which signals the pituitary to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH then stimulates the testes to produce testosterone, while FSH is crucial for sperm production. When synthetic testosterone is introduced, the brain interprets high levels of this hormone, reducing the output of GnRH, LH, and FSH. This leads to a decline in natural testosterone synthesis, a condition known as hypogonadism.
- Hypothalamus: Reduces GnRH release.
- Pituitary Gland: Decreases LH and FSH production.
- Testes: Undergo atrophy due to lack of stimulation, significantly impairing natural testosterone and sperm production.
This suppression isn’t always temporary. Depending on the duration and dosage of steroid use, the HPG axis can be significantly damaged, leading to prolonged or even permanent dysfunction. Individuals often experience a period of severe hypogonadism after discontinuing steroids, commonly referred to as “post-cycle therapy” (PCT) in the bodybuilding community, where they attempt to restore natural function, often with limited success. The impact on physical and psychological well-being during this phase can be profound.
Understanding this fundamental disruption is key to grasping the cascade of sexual health problems that follow. It’s not merely about “bouncing back” after a cycle; the body’s intricate hormonal machinery is designed for precision and balance, which steroids brutally undermine. This initial hormonal disarray sets the stage for many of the issues we will explore.
erectile dysfunction and libido impairment
One of the most immediate and distressing long-term effects of steroid use on male sexual health is the development of erectile dysfunction (ED) and a significant reduction in libido. While some users might initially experience an increase in libido due to supraphysiological testosterone levels, this effect often reverses as the body’s natural production is suppressed or as steroid cycles conclude. The relationship between testosterone and erectile function is complex, involving direct effects on penile tissues and indirect effects on mood, energy, and sexual desire.
Chronic suppression of natural testosterone production, known as hypogonadism, is a primary culprit behind steroid-induced ED. Testosterone is essential for maintaining healthy erectile function, as it influences the nitric oxide pathway in the penis, which is crucial for vasodilation and blood flow necessary for an erection. When natural testosterone levels plummet, this mechanism is compromised, leading to difficulties in achieving or maintaining an erection. Moreover, psychological factors often play a significant role; the anxiety and stress associated with performance issues can exacerbate ED, creating a vicious cycle.
the dual impact on erection and desire
The impact extends beyond the physical ability to achieve an erection; it also deeply affects sexual desire. Libido, or sex drive, is highly dependent on adequate testosterone levels. Low testosterone can lead to a general lack of interest in sex, reduced fantasies, and decreased responsiveness to sexual stimuli. This can have far-reaching implications for relationships and overall quality of life.
- Physical ED: Compromised blood flow and signaling due to low natural testosterone.
- Psychological Distress: Anxiety, depression, and self-esteem issues stemming from sexual performance problems.
- Libido Crash: Markedly reduced sex drive and interest, often persisting long after steroid cessation.
Many steroid users report a temporary “boost” in libido during a cycle, but this is often followed by a severe crash once exogenous hormones are withdrawn or when the body’s natural production fully shuts down. This creates a dependency, as users might feel compelled to continue taking steroids simply to maintain some semblance of sexual function and desire, trapping them in a cycle of abuse. The psychological toll of these changes should not be underestimated, as it often leads to depression, anxiety, and relationship difficulties, further complicating recovery.
Addressing steroid-induced ED and libido impairment often requires a multi-faceted approach, including restoring natural hormonal balance, if possible, and addressing the underlying psychological impacts. However, the path to full recovery can be long and uncertain, highlighting the severe and often persistent nature of these long-term consequences.

infertility and testicular atrophy
The concept of fertility is deeply intertwined with a man’s reproductive health, and anabolic steroid use presents a significant threat to this critical aspect of well-being. Testicular atrophy and infertility are among the most common and often irreversible long-term consequences of prolonged steroid abuse. As discussed, the suppression of the HPG axis directly interferes with the testes’ ability to produce testosterone and, crucially, sperm. The testes, deprived of the necessary stimulatory hormones (LH and FSH), shrink in size – a phenomenon known as testicular atrophy.
This atrophy is not merely cosmetic; it is a clear indicator of impaired testicular function. When the testes shrink, their capacity for spermatogenesis (sperm production) is severely compromised. Many steroid users, especially those on long-term, high-dose cycles, experience azoospermia (complete absence of sperm in semen) or oligospermia (very low sperm count). This can lead to significant fertility issues, making it difficult or impossible to conceive a child naturally. The impact of this on personal life and family planning can be devastating, underscoring the profound and intimate consequences of steroid abuse.
reversibility and rehabilitation challenges
The reversibility of testicular atrophy and infertility varies greatly among individuals, depending on factors such as the duration and dosage of steroid use, the specific type of steroids used, and individual physiological responses. While some men may regain partial or full fertility after discontinuing steroids and undergoing post-cycle therapy, for many, the damage can be permanent. This uncertainty adds another layer of distress for those attempting to recover from steroid abuse.
- Testicular Shrinkage: Visible and palpable reduction in testicular size due to suppression.
- Sperm Production Impairment: Leading to azoospermia or oligospermia, severely impacting fertility.
- Variable Recovery: Fertility may or may not return, even with medical intervention.
Medical interventions post-steroid use often involve hormone replacement therapies (HRT) or selective estrogen receptor modulators (SERMs) to try and kickstart natural testosterone and sperm production. However, these treatments are not always successful, and the journey to recovery can be prolonged and emotionally taxing. The psychological burden of potential permanent infertility can be immense, affecting self-esteem, relationships, and future life choices. It highlights the profound and often overlooked long-term risks associated with the pursuit of a temporary physical ideal. The discussion around potential permanent damage is critical, as many users underestimate this aspect.
For young men considering steroid use, the irreversible potential for infertility should be a major deterrent. The short-term gains in muscle mass pale in comparison to the potential loss of the ability to father children. This deep dive into the physiological mechanisms behind testicular atrophy and infertility underscores the hidden dangers that extend far beyond aesthetics.
gynecomastia and other physical changes
Beyond the internal hormonal chaos, anabolic steroid use often manifests in visible and deeply distressing physical changes, with gynecomastia being one of the most well-known. Gynecomastia is the development of excess breast tissue in males, leading to enlarged breasts that can range from a subtle puffiness under the nipple to fully developed, feminine-looking breasts. This occurs because the body, in an attempt to metabolize the excess synthetic testosterone, often converts it into estrogen through an enzyme called aromatase. High estrogen levels then stimulate the growth of mammary gland tissue, similar to how breast development occurs in females.
While often benign from a health perspective, gynecomastia can be incredibly psychologically distressing for men, particularly those who began steroid use to enhance their masculinity. The irony of developing female breast tissue while seeking a more masculine physique is not lost on users, leading to severe body image issues, embarrassment, and social anxiety. In some cases, the enlarged breast tissue can also be painful or tender to the touch. Surgical removal is often the only effective treatment for established gynecomastia, representing a permanent and costly consequence.
skin, hair, and voice alterations
The androgenic component of steroids also drives a range of other physical changes. These can include severe acne, particularly on the face, back, and chest, resulting from increased sebum production. Hair loss, specifically male pattern baldness, can be accelerated, even in individuals not genetically predisposed to early hair thinning. Paradoxically, some men may experience increased body hair growth. These changes, while not directly involving sexual organs, contribute to the overall negative body image and psychological distress associated with long-term steroid use.
- Gynecomastia: Enlarged male breast tissue due to estrogen conversion.
- Acne: Severe breakouts on the face, back, and chest.
- Hair Loss/Growth: Accelerated male pattern baldness and increased body hair.
Another less common but irreversible change reported by some long-term users is a deepening of the voice. This is due to the thickening of the vocal cords, a permanent effect of androgen exposure. While often associated with female steroid users, it can occur in males who experience extreme androgenic effects. These visible changes, coupled with the internal health issues, create a profound and often humiliating alteration in a man’s physical presentation, severely impacting his self-perception and how he interacts with the world. The psychological burden of these changes can be significant, leading to further isolation and mental health issues. Managing these physical changes often involves dermatological treatments for acne and, as mentioned, surgical intervention for gynecomastia, both of which carry their own risks and costs.
psychological and emotional impacts
The long-term effects of steroid use on male sexual health extend far beyond physiological changes, deeply impacting psychological and emotional well-being. The pursuit of an idealized physique often comes at the cost of mental stability, creating a complex interplay between body image, performance anxiety, and mood disorders. The hormonal fluctuations inherent in steroid cycles – from the initial high levels of synthetic testosterone to the plummeting natural levels during post-cycle recovery – can trigger significant mood swings, irritability, aggression, and even episodes of clinical depression.
Users often report heightened aggression, famously dubbed “roid rage,” which can lead to strained relationships, impulsivity, and even violence. While these extreme manifestations may subside post-cycle, a more insidious form of emotional dysregulation can persist. The profound impact on sexual function, including ED and decreased libido, frequently leads to feelings of shame, inadequacy, and a loss of self-esteem. This can manifest as social withdrawal, avoidance of intimate situations, and a pervasive sense of failure, which further exacerbates depressive symptoms. The irony is that men often turn to steroids to enhance their confidence and attraction, only to find themselves emotionally crippled and sexually dysfunctional.
body dysmorphia and dependency
A significant psychological component often fueling steroid abuse is muscle dysmorphia, a condition where an individual perceives themselves as significantly smaller or less muscular than they actually are, despite possessing a well-developed physique. This distorted body image can drive continued steroid use, even in the face of obvious negative consequences, leading to psychological dependency. Users become trapped in a relentless pursuit of an unattainable ideal, constantly comparing themselves to others and feeling inadequate.
- Mood Swings: Rapid shifts between irritability, aggression, and depressive states.
- Anxiety and Depression: Chronic feelings of worry, sadness, loss of pleasure, particularly post-cycle.
- Body Dysmorphia: Distorted perception of one’s own body, leading to compulsive behaviors.
- Psychological Dependency: Feeling unable to cope without steroids, even with their negative effects.
The cycle of steroid use often becomes intertwined with mental health struggles. The initial “high” from perceived gains can mask underlying insecurities, but as side effects mount and natural hormonal function declines, these insecurities intensify. The physical changes, such as gynecomastia or hair loss, further compound body image issues, creating a sense of self-loathing. The secretive nature of steroid abuse can also lead to isolation, as users may hide their habits from friends and family, further contributing to feelings of loneliness and despair. Effective recovery from steroid use often requires addressing these deep-seated psychological issues through therapy, support groups, and, in some cases, psychiatric intervention to manage depression and anxiety, highlighting that the damage isn’t just physical.
cardiovascular and systemic health risks
While the focus here is on sexual health, it is imperative to acknowledge that the long-term use of anabolic steroids poses significant dangers to overall physiological health, particularly affecting the cardiovascular system. Steroids can profoundly alter lipid profiles, leading to increased levels of low-density lipoprotein (LDL or “bad” cholesterol) and decreased levels of high-density lipoprotein (HDL or “good” cholesterol). This adverse shift significantly increases the risk of atherosclerosis, a condition where plaque builds up inside the arteries, narrowing them and making them less flexible, which can lead to heart attack and stroke.
Furthermore, steroid use is associated with elevated blood pressure and an increased risk of developing cardiomyopathy, a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body, potentially leading to heart failure. The liver, being the primary organ for metabolizing steroids, is also highly vulnerable. Long-term oral steroid use, in particular, can lead to liver damage, including peliosis hepatis (blood-filled cysts) and even liver tumors. These systemic risks underscore that the body’s systems are interconnected; damage in one area inevitably impacts others, compounding the overall health burden.
beyond the primary systems
The reach of steroid-induced damage extends even further, impacting various other bodily systems. The kidneys can be strained, leading to kidney disease. The immune system can be compromised, making users more susceptible to infections. Musculoskeletal issues, contrary to the muscle-building intent, can also arise; while bulk is gained, the connective tissues (tendons and ligaments) may not strengthen at the same rate, increasing the risk of tears and injuries. The bone structure can also be affected, though this is more complex and less uniformly reported.
- Cardiovascular Damage: Increased LDL, decreased HDL, high blood pressure, cardiomyopathy, increased risk of heart attacks and strokes.
- Liver Toxicity: Liver damage, cysts, and tumors, especially with oral steroids.
- Kidney Strain: Potential for kidney disease due to metabolic stress.
- Musculoskeletal Imbalance: Increased risk of tendon and ligament injuries.
The interconnectedness of these systems means that dysfunction in one area, such as compromised cardiovascular health, can indirectly affect sexual health through impaired blood flow or overall reduced vitality. For instance, poor cardiovascular health contributes to erectile dysfunction. This holistic view of the body is crucial when discussing the perils of steroid use. The pursuit of superficial gains often ignores the profound internal damage, creating a ticking time bomb of health problems that can manifest years down the line, ultimately diminishing quality of life and longevity. The multi-systemic impact of these drugs means that no part of the body remains unaffected, making the decision to use them a gamble with very high stakes.
prevention, recovery, and seeking help
Understanding the severe long-term effects of steroid use on male sexual health, along with systemic risks, naturally leads to the crucial discussion of prevention and recovery. The most effective strategy is, unequivocally, prevention. Education plays a vital role in dispelling myths surrounding steroid use, particularly among younger populations susceptible to body image pressures and the allure of quick physical transformation. Open dialogue about the irreversible damage to fertility, sexual function, and overall health can serve as a powerful deterrent. Promoting healthy body image, emphasizing the value of natural physical development, and highlighting the dangers of performance-enhancing drugs are essential components of public health initiatives.
For those already engaged in steroid use, the path to recovery is challenging but necessary. The first step involves discontinuing steroid use, often under medical supervision. The “post-cycle crash” can be extremely difficult, marked by severe hypogonadism, depression, and loss of muscle mass, which often pushes individuals back to steroid use. Medical professionals specializing in addiction and endocrinology can provide crucial support, including hormone replacement therapy (HRT) or selective estrogen receptor modulators (SERMs) to help stabilize the hormonal system and mitigate withdrawal symptoms. However, it’s important to manage expectations, as the body’s natural hormonal balance may not fully recover, especially after prolonged or high-dose usage.
the role of therapy and support systems
Beyond the physical aspects, psychological support is paramount. Therapy, especially cognitive-behavioral therapy (CBT), can help address underlying issues such as body dysmorphia, low self-esteem, and the psychological dependency on steroids. Support groups, where individuals can share experiences and strategies for recovery, provide a crucial sense of community and reduce feelings of isolation. Family and friends also play a critical role, offering understanding, encouragement, and holding individuals accountable for their recovery journey.
- Education: Informing about risks, especially for young individuals.
- Medical Supervision: Guidance for safe discontinuation and managing withdrawal.
- Hormonal Therapy: Prescribed treatments to aid hormonal balance restoration.
- Psychological Support: Therapy (CBT) and support groups for mental and emotional recovery.
- Holistic Well-being: Focusing on nutrition, exercise, and mental health for overall recovery.
The recovery process is not linear and requires immense commitment. Relapses are possible, but each attempt to recover is a step towards better health. Emphasizing a holistic approach to well-being, including balanced nutrition, regular natural exercise, and mental health practices, can significantly aid recovery. The long-term impact on sexual health, while distressing, should serve as a powerful motivator for seeking help. Reassurance that recovery is possible, even if complete functionality isn’t always restored, can provide hope. The journey back to natural health and well-being, while arduous, is ultimately far more rewarding than the temporary and damaging gains offered by steroids, promoting a life of genuine health and self-acceptance.
| Key Effect | Brief Description |
|---|---|
| 🔄 Hormonal Imbalance | Suppression of natural testosterone production, leading to hypogonadism. |
| 🍆 Erectile Dysfunction | Difficulty achieving or maintaining erections due to low natural testosterone. |
| 📉 Infertility & Atrophy | Reduced sperm count/absence of sperm and shrunken testes. |
| 🧠 Psychological Distress | Mood swings, depression, anxiety, and body dysmorphia. |
Frequently Asked Questions About Steroids and Male Sexual Health
Long-term steroid use can indeed lead to permanent erectile dysfunction (ED) due to persistent suppression of the body’s natural testosterone production. While some individuals may regain partial function after cessation and medical intervention, severe or prolonged abuse can cause irreversible damage to the hormonal axis, making full recovery of erectile function uncertain.
Steroid use can cause temporary or, in many cases, permanent infertility. The suppression of sperm production can be severe, leading to azoospermia. While fertility may return for some after stopping steroids and undergoing treatment, the duration and dosage of use significantly impact reversibility. For many, the damage is irreversible, resulting in lasting infertility.
“Roid rage” refers to extreme mood swings and aggressive outbursts associated with steroid use. This heightened irritability and aggression can severely strain sexual relationships by fostering an environment of fear or discomfort, reducing intimacy, and leading to arguments, ultimately diminishing sexual desire and connection between partners.
Gynecomastia, or male breast enlargement, caused by steroid use is often not fully reversible through natural means or post-cycle therapy. While some minor cases might improve, established breast tissue growth usually requires surgical removal to achieve a flat chest. This procedure is the most effective way to eliminate the excess glandular and fatty tissue.
The duration of sexual side effects after stopping steroids varies widely. Some individuals may experience symptoms for months, while others could face permanent issues. Factors like duration and dosage of use, individual physiology, and any concurrent medical treatments influence recovery time. Full restoration of natural sexual health can be a lengthy process, often requiring significant medical intervention and lifestyle changes.
Conclusion
The journey through the long-term effects of steroid use on male sexual health reveals a sobering reality: what begins as a quest for physical enhancement often culminates in profound and lasting damage to one’s most intimate well-being. From the intricate hormonal disruptions leading to erectile dysfunction and permanent infertility, to the visible and distressing physical changes like gynecomastia, and the insidious erosion of psychological health, the consequences are far-reaching. The scientific evidence consistently points to a complex array of risks that extend well beyond the initial allure. Recognizing these dangers is not just about avoiding harm, but about promoting a healthier, more authentic approach to well-being that values sustained health over fleeting physical ideals. Ultimately, prioritizing natural physical development, educating oneself, and seeking professional help for body image concerns or substance abuse are the most empowering steps a man can take for his present and future health.





