PTSD in Men: Symptoms, Causes, and Treatments Explained
Post-traumatic stress disorder (PTSD) manifests uniquely in men, often presenting through irritability, anger, and avoidance behaviors, stemming from various traumatic experiences, necessitating a comprehensive understanding of its symptoms, underlying causes, and effective therapeutic interventions for proper diagnosis and recovery.
Understanding PTSD in men: symptoms, causes, and effective treatments is crucial, as post-traumatic stress disorder often presents differently in men than in women, leading to misdiagnosis or delayed recognition. This guide aims to shed light on the nuances of PTSD in the male population, exploring the unique ways it manifests, the underlying factors contributing to its development, and the most effective strategies for treatment and recovery.
The Silent Struggle: Recognizing PTSD Symptoms in Men
Post-traumatic stress disorder is a complex mental health condition that can develop after a person experiences or witnesses a terrifying event. While the core criteria for diagnosis are universal, the way PTSD manifests can vary significantly between individuals. In men, symptoms often present in ways that are less overtly emotional and more behavioral, which can make identification challenging.
One common presentation in men is an increase in irritability and aggression. Rather than expressing sadness or fear directly, men might lash out at loved ones or engage in risky behaviors. This outward display of anger can often mask the internal turmoil of flashbacks, intrusive thoughts, or emotional numbness. Understanding these subtle, often internalized, signs is the first step toward effective intervention.
Common Behavioral Indicators of PTSD in Men
Men with PTSD may exhibit a range of behavioral changes, which are often coping mechanisms for overwhelming internal distress. These behaviors, while seemingly disparate, often serve to either numb intense emotions or regain a sense of control that was lost during the traumatic event. It’s important to recognize that these actions are not character flaws but rather symptoms of a deeper struggle.
- Increased substance use: Turning to alcohol or drugs to self-medicate and escape painful memories or intense emotional states.
- Risk-taking behaviors: Engaging in dangerous activities, such as reckless driving or extreme sports, possibly as a way to feel alive or regain a sense of control.
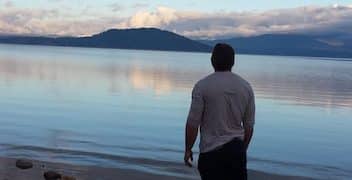
- Social isolation: Withdrawing from friends, family, and activities they once enjoyed, often due to feelings of detachment or a fear of judgment.
- Workaholism: Burying themselves in work to avoid dwelling on traumatic experiences or to maintain a sense of purpose and routine.
These behaviors can lead to significant problems in relationships, employment, and overall well-being. Recognizing them as potential indicators of PTSD is vital for encouraging men to seek help.
Emotional and Cognitive Manifestations
Beyond behavioral shifts, men with PTSD also experience significant emotional and cognitive disruptions. These are often more internalized and can be harder for others to notice, but they are profoundly impactful on the individual’s inner world. Cognitive symptoms often include difficulty concentrating or memory problems, which can impede daily functioning and decision-making.
Emotional numbness, also known as emotional blunting, is another pervasive symptom. This can involve an inability to experience positive emotions, a feeling of detachment from others, or a general sense of apathy. This blunting can lead to misunderstandings with partners and family, who may perceive it as a lack of caring. Similarly, persistent negative beliefs about oneself, others, or the world are common, such as feeling that no one can be trusted or that the world is inherently dangerous.
Nightmares and sleep disturbances are also frequent, robbing individuals of restorative sleep and exacerbating other symptoms. These pervasive symptoms underscore the need for a nuanced understanding of how PTSD affects men.
The Roots of Trauma: Exploring Causes of PTSD in Men
While PTSD can stem from a wide array of traumatic events, certain types of experiences are more commonly associated with its development in men. Understanding these prevalent causes can help in identifying at-risk individuals and tailoring preventative measures or early interventions. The unique societal expectations often placed on men can also influence how they perceive and react to trauma.
Combat exposure is perhaps the most widely recognized cause of PTSD in men, given the historical context of military service. However, it’s far from the only, or even always the primary, root. Other significant traumatic events include violent crime, accidents, natural disasters, and childhood abuse. Each of these can leave a profound psychological imprint that develops into PTSD.
Military Combat and Service-Related Trauma
For decades, military combat has been a leading cause of PTSD among men. Soldiers in active combat zones are exposed to extreme violence, constant threat, and often witness horrific events, including death and severe injury. The cumulative effect of these experiences can be devastating, leading to profound psychological wounds that persist long after their return home.
Beyond active combat, other service-related traumas can trigger PTSD. These include military sexual trauma (MST), training accidents, or even the stress of deployment and separation from family. The culture within the military, which often emphasizes stoicism and mental toughness, can also inadvertently discourage service members from processing their emotions or seeking help, thereby increasing the risk of PTSD long-term. This suppression can make the eventual presentation of symptoms more explosive or internalized years later.
The transition back to civilian life can also be a significant challenge, as veterans often struggle to reintegrate into a society that may not fully comprehend their experiences. This lack of understanding can exacerbate feelings of isolation and alienation, further complicating recovery from service-related PTSD.
Non-Military Traumatic Events
Beyond military service, men are susceptible to PTSD from a variety of other traumatic experiences. These events, while perhaps less frequently discussed in the context of men’s mental health, are equally capable of causing severe psychological distress. Such traumas often challenge a man’s sense of safety, control, and personal agency, leading to lasting impacts.
- Violent crime: Being a victim of assault, robbery, or other violent acts can shatter a man’s sense of security and lead to hypervigilance and fear.
- Serious accidents: Car crashes, industrial accidents, or natural disasters can result in profound shock and a feeling of helplessness, contributing to PTSD.
- Childhood abuse or neglect: Experiences of physical, emotional, or sexual abuse during formative years can have long-lasting effects, manifesting as PTSD in adulthood.
- Sudden, unexpected death or severe injury of a loved one: Witnessing or being closely involved in such events can be deeply traumatizing.
The impact of non-military trauma can be just as profound as combat trauma, and recognition of these diverse causes is essential for accurate diagnosis and compassionate care.

Paths to Healing: Effective Treatments for PTSD in Men
The journey to recovery from PTSD in men, though challenging, is absolutely possible with the right therapeutic approaches and support systems. Effective treatment typically involves a combination of psychotherapy, sometimes augmented by medication, and a strong emphasis on building healthy coping mechanisms and support networks. The key is finding approaches that resonate with the individual’s needs and preferences, acknowledging the unique ways men might engage with treatment.
The goal of treatment is not simply to “forget” the trauma, but rather to process the memories and emotions in a safe environment, reducing their power and enabling the individual to reclaim their life. This often involves reducing avoidance behaviors, confronting distressing thoughts, and developing resilience.
Evidence-Based Psychotherapies
Several psychotherapeutic approaches have proven highly effective in treating PTSD. These therapies provide structured frameworks for processing trauma and developing coping skills, helping men to regain a sense of control over their thoughts and emotions. The efficacy of these treatments is supported by extensive research, making them first-line interventions.
Cognitive Behavioral Therapy (CBT), particularly its trauma-focused variations, is a cornerstone of PTSD treatment. CBT helps individuals identify and challenge distorted thoughts and beliefs related to the trauma, leading to more realistic and less distressing interpretations. Techniques such as exposure therapy, where individuals gradually and safely confront feared memories or situations, are often integrated into CBT. This systematic approach allows for desensitization and reduction in avoidance behaviors that maintain PTSD symptoms.
Eye Movement Desensitization and Reprocessing (EMDR) therapy is another highly effective treatment. EMDR involves guiding the patient to process traumatic memories while simultaneously engaging in rhythmic eye movements or other bilateral stimulation. This process is believed to help the brain reprocess traumatic memories, reducing their emotional impact and allowing for resolution. Many men find EMDR a less direct confrontation of their emotions, which can be appealing.
Prolonged Exposure (PE) therapy involves confronting trauma-related thoughts, feelings, and situations that have been avoided. This is done gradually and systematically, with the goal of reducing the fear and distress associated with these triggers. PE includes both in-vivo exposure (facing real-life feared situations) and imaginal exposure (repeatedly recounting the traumatic memory).
Medication and Adjunctive Therapies
While psychotherapy is often the primary treatment for PTSD, medication can play a critical role, particularly in managing severe symptoms that interfere with daily functioning or engagement in therapy. Antidepressants, specifically selective serotonin reuptake inhibitors (SSRIs), are commonly prescribed to alleviate symptoms such as depression, anxiety, and irritability often accompanying PTSD. These medications can help stabilize mood and reduce the intensity of intrusive thoughts and nightmares, thereby making psychotherapy more accessible and effective.
Beyond traditional medication, adjunctive therapies and complementary approaches can provide additional support and help men develop broader coping strategies. Mindfulness-based stress reduction, for instance, teaches techniques to stay present and observe thoughts and feelings without judgment, which can be particularly helpful for managing intrusive thoughts and flashbacks. Similarly, yoga and other forms of physical activity can help to regulate the nervous system, reduce tension, and improve sleep quality, all of which contribute to overall well-being and recovery.
Support groups, tailored specifically for men or for individuals with similar traumatic experiences (e.g., military veterans), offer invaluable peer support. Sharing experiences with others who understand can reduce feelings of isolation and provide a sense of community, fostering an environment where men feel safe to express their vulnerabilities and learn from one another’s coping strategies.
Addressing Stigma: Why Men Often Don’t Seek Help
The path to recovery from PTSD is often complicated by societal pressures and deeply ingrained stereotypes about masculinity. Men are frequently encouraged to be strong, self-reliant, and stoic, leading to a pervasive stigma around seeking mental health support. This cultural narrative can make it incredibly difficult for men to admit vulnerability, express distress, or acknowledge the need for professional help, even when they are suffering profoundly from PTSD.
The fear of being perceived as weak, a burden, or less “manly” can be a formidable barrier. This reluctance to open up often leads to internalizing symptoms, which can manifest as anger, substance abuse, or social withdrawal, further complicating diagnosis and delaying treatment. Breaking down these systemic and self-imposed barriers is critical for improving outcomes for men with PTSD.
Societal Pressures and Masculinity Norms
Traditional notions of masculinity often dictate that men should be resilient, unemotional, and capable of handling their own problems without assistance. These expectations, while seemingly benign, create an environment where emotional expression is discouraged and seeking help for mental health issues is viewed as a sign of weakness. This cultural pressure runs deep, influencing how men perceive their own distress and their willingness to seek support. The impact of such norms on mental health can be profound, especially after experiencing trauma.
Often, men internalize these messages, believing that they should “tough it out” or that their emotional struggles are a personal failing. This can lead to a cycle of shame and isolation, as they hide their symptoms from friends, family, and even themselves. The societal ideal of the “strong, silent type” can be particularly damaging when applied to psychological trauma, as it directly contradicts the need for open communication and emotional processing that is essential for recovery from PTSD. Overcoming these entrenched beliefs requires ongoing education and a shift in cultural narratives to embrace emotional resilience as a strength.
The media’s portrayal of men, often emphasizing physical strength and emotional detachment, further reinforces these norms. This creates a challenging environment for men to feel comfortable expressing vulnerability, thus perpetuating the cycle of silence surrounding mental health struggles.
The Impact of Stigma on Diagnosis and Treatment
The pervasive stigma surrounding mental health issues, particularly for men, has direct and detrimental consequences on both diagnosis and treatment. When men feel compelled to mask their symptoms, healthcare providers may misinterpret their distress or fail to recognize PTSD altogether. Symptoms like increased irritability, anger, or substance use might be dismissed as character flaws or behavioral issues rather than signs of a treatable condition. This misinterpretation can lead to delayed diagnosis, protracted suffering, and, in some cases, the development of co-occurring conditions like depression or addiction, further complicating recovery.
Furthermore, even when a diagnosis is made, stigma can prevent men from adhering to treatment plans. Fear of judgment from peers, family, or employers can lead to reluctance in attending therapy sessions, openly discussing their experiences, or taking prescribed medications. The desire to maintain a façade of strength can override the clear benefits of professional intervention, leading to a fragmented and less effective treatment journey. Addressing and dismantling these stigmatizing beliefs is not just a societal goal but a critical step in ensuring men receive the timely and appropriate care they need for PTSD.
Educating the public, healthcare providers, and men themselves about PTSD and its diverse manifestations is essential. Creating safe and supportive environments where men feel empowered to seek help without fear of reprisal or judgment is paramount to improving outcomes.
Building Resilience: Proactive Strategies for Men’s Mental Health
Beyond treatment for existing PTSD, proactive strategies and healthy coping mechanisms are vital for building resilience and preventing relapse in men. These strategies focus on empowering individuals with tools to manage stress, process emotions effectively, and maintain overall well-being. Cultivating a supportive environment, both personally and professionally, plays a significant role in fostering mental health resilience.
Engaging in regular physical activity, practicing mindfulness, and nurturing strong social connections are all powerful components of a comprehensive resilience-building plan. These elements work synergistically to enhance emotional regulation, reduce the physical symptoms of stress, and provide a buffer against future traumatic events.
Developing Healthy Coping Mechanisms
Developing healthy coping mechanisms is fundamental for managing the ongoing challenges associated with PTSD and for building resilience against future stressors. These mechanisms empower men to navigate difficult emotions and intrusive thoughts constructively, rather than resorting to avoidance or destructive behaviors. Cultivating a diverse set of coping tools ensures flexibility in responding to various triggers and challenges.
- Regular physical activity: Exercise can be a powerful stress reliever and mood booster, helping to regulate emotions and improve sleep.
- Mindfulness and meditation: Practicing mindfulness can help men stay present, reduce rumination, and cultivate a sense of calm amidst inner turmoil.
- Engaging in hobbies and interests: Pursuing enjoyable activities provides a healthy distraction, fosters a sense of accomplishment, and allows for positive emotional experiences.
- Journaling: Writing down thoughts and feelings can be a private and effective way to process emotions, identify patterns, and gain perspective on traumatic experiences.
These strategies, when consistently applied, can significantly enhance an individual’s capacity to cope with trauma-related symptoms and improve overall mental well-being, fostering a stronger foundation for long-term recovery.

The Importance of Social Support Networks
A robust social support network is an indispensable component of healing and resilience for men grappling with PTSD. Isolation, often a symptom and a consequence of trauma, can exacerbate feelings of loneliness and despair. Conversely, meaningful connections with others provide a crucial buffer against these negative emotions, offering empathy, understanding, and practical assistance. For men, who may feel pressured to project an image of self-sufficiency, having a trusted circle where they can be genuinely vulnerable without judgment is transformative.
This network can include family, friends, support groups, or even online communities. The act of sharing experiences with others who have faced similar challenges can validate feelings, reduce shame, and foster a sense of belonging. Furthermore, a strong support system can encourage men to seek and adhere to professional treatment, serving as an accountability partner and a source of encouragement during difficult times. The reciprocal nature of support, where one both receives and provides care, strengthens bonds and reinforces a sense of purpose.
Ultimately, nurturing and leaning on a reliable social network is not a sign of weakness but a testament to personal strength and a wise investment in long-term mental health. It provides a foundational safety net, enabling men to navigate the complexities of PTSD with greater confidence and hope.
| Key Point | Brief Description |
|---|---|
| 😠 Unique Symptoms | Men often exhibit irritability, anger, and avoidance behaviors rather than overt sadness or fear. |
| ⚔️ Diverse Causes | Beyond combat, PTSD in men stems from violent crime, accidents, abuse, and bereavement. |
| 💡 Effective Treatments | Psychotherapies like CBT and EMDR, often combined with medication, are highly effective. |
| 🗣️ Overcoming Stigma | Societal pressures against male emotional expression delay diagnosis and treatment. |
Frequently Asked Questions About PTSD in Men
In men, PTSD often manifests as externalized behaviors such as irritability, anger, substance abuse, and risk-taking. Compared to women, who might exhibit more internalizing symptoms like anxiety and depression, men may express hyperarousal through aggression or emotional numbness, making it harder to recognize typical PTSD signs.
While combat exposure is a significant cause, men can develop PTSD from various traumatic experiences. These include violent crimes (assault, robbery), serious accidents, natural disasters, and childhood physical or sexual abuse. Witnessing the unexpected death or severe injury of a loved one can also be a profound trigger for PTSD in men.
Evidence-based psychotherapies are highly effective. These include Cognitive Behavioral Therapy (CBT), especially Trauma-Focused CBT and Prolonged Exposure (PE), which help process traumatic memories. Eye Movement Desensitization and Reprocessing (EMDR) therapy is also widely used. Medication, such as SSRIs, can manage severe symptoms and facilitate therapeutic engagement.
Societal norms surrounding masculinity often dictate that men should be self-reliant and emotionally stoic, making it challenging to admit vulnerability. This stigma leads to fear of judgment or appearing weak, causing men to internalize symptoms and avoid professional help, thus delaying diagnosis and treatment for their PTSD.
Strong social support networks provide a safe space for men to express emotions and share experiences, reducing feelings of isolation and shame linked to PTSD. Connecting with understanding friends, family, or support groups can validate their experiences, reinforce positive coping mechanisms, and encourage consistent engagement in treatment, crucial for long-term recovery.
Conclusion: Empowering Men on the Path to Healing
Understanding PTSD in men, from its varied symptoms and root causes to the most effective treatments, is not merely an academic exercise; it is a critical step toward fostering resilience and promoting healing. By recognizing the unique ways PTSD manifests in men, challenging societal stigmas, and promoting accessible, evidence-based interventions, we can empower men to seek the help they deserve. The journey to recovery is deeply personal, yet it is fortified by compassion, expert guidance, and robust support systems. Moving forward requires a collective commitment to creating environments where men feel safe to acknowledge their struggles and embark on the path to reclaiming their lives from the shadows of trauma.